Deleshia D. Kinney, MD,MPH, MAT, affectionately known to friends and family as Dr. Dyi, first discovered she had high blood pressure when she was in medical school. “We would play around with the blood pressure monitor, taking each other’s blood pressure,” she said. One day, a fellow student pointed out to Dr. Dyi that her blood pressure was high. “No way,” was her first reaction. But when her doctor confirmed it, she accepted the inevitable. After all, it ran in her family. “My mother and grandmother had it,” she said, “But my grandmother never had a stroke. My mother did. I was put on medication, right away.”
According to the Office of Minority Health, “Although African American adults are 30 percent more likely to have high blood pressure, they are less likely than non-Hispanic whites to have their blood pressure under control. African American women are nearly 50 percent more likely to have high blood pressure, as compared to non-Hispanic white women.” Dr. Dyi made the necessary lifestyle changes to keep her blood pressure under control. As a public health practitioner, she knew what to do. “I ate the right foods, exercised every day, got good sleep, and took my blood pressure medication.”
Then her father passed, and she, her son and her brother went to his home country of Ghana. “When I got home, my blood pressure medication was running out,” she said. Indeed, by the time she returned to the states she was completely out of her medication. “After spending a month in Ghana, I had a lot to do to get things together at home,” she explained, “I kept putting off getting a new prescription for my medication. I kept saying, ‘I’ll get around to it.“
She hadn’t gotten around to it on the day a guy friend stopped by the house. “He asked if I wanted him to get me something to eat and I said ‘sure,’ but I wasn’t really hungry,” she said. “Then he came back with Sushi. I love Sushi, but I didn’t eat any of it.” Sensing something was wrong, he repeatedly asked if she was okay, and she repeatedly assured him she was. “But as I told him I was okay, I wished he could see what I was seeing,” she said, “I was reading, and the words were falling off the paper.” For some reason, she didn’t find it unusual that she asked him to help her to the bathroom, and after she stayed in the bathroom too long and he again inquired if she was okay, she asked him to come and help her get back to the couch. “I still wasn’t convinced that I was sick,” she said, “But about eight o’clock, when I went to lay down, he knew something was wrong. He ignored me and decided to call the doctor.” I had all the symptoms.
She remembered going to the hospital, but the last thing she remembered was him placing her on the hospital bed. Three days later, she woke up. “Nothing hurt,” she said, “It wasn’t scary. But then I tried to talk, and no one could understand me. And then I tried to move, and that’s when I realized it might have been a little more than I thought it was.” The doctor told her she had a stroke. “I thank God that so many people came to see me,” she said, “It wasn’t bad as far as being painful. It’s just realizing you can’t do the things you used to do.”
Dr. Dyi knows that if she had gotten to the hospital sooner, if her friend had known the signs, it might have stopped her from having a full-blown stroke. “First, get them to the hospital right away. If you’re having symptoms, if you feel like something is wrong, call 911. Get to the doctor immediately.”
The mnemonic F.A.S.T. can be used as a quick test to determine stroke:
F – Face drooping: Ask the person to smile and see if their smile is uneven or if their face droops to one side.
A – Arm weakness: Ask the person to raise both arms to see if one arm is weak, numb, or drifts downward.
S – Speech difficulty: Ask the person to speak to see if their speech is slurred.
T – Time to call 911: Do not drive to the hospital or let someone else drive you. Call 911 for an ambulance to begin treatment right away.
A stroke can happen to anyone at any age. The older you are, your chances of having a stroke are increased.
However, people younger than 65 also have strokes. About one in seven strokes happen to people ages 15 to 49, according to the CDC. Dr. Dyi was 47.
There are some risk factors you can’t control, such as age, family history, or gender. But there are some common medical conditions and lifestyle habits that put you more at risk for stroke. These include high blood pressure, high cholesterol, diabetes, being overweight, smoking, and not exercising enough, to name a few.
Dr. Dyi recuperated well from her stroke, and she attributes that to the fact that she was eating right, exercising, and sleeping well. She also engages in intermediate fasting. “On those days, I won’t eat until one o’clock pm and then I stop at eight o’clock pm.” However, the fact that she was observing a healthy lifestyle may also be the reason that she felt comfortable skipping her medication. She is convinced that skipping her medication was the only reason she had a stroke.
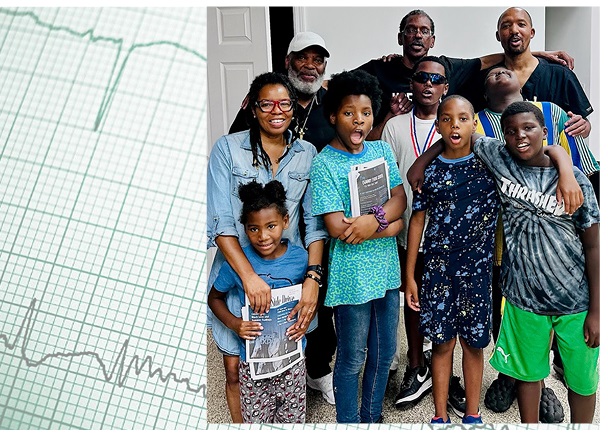
“I am a stroke success,” Dr. Dyi says. She is indeed. According to a Harvard Medical School report, “Strokes can be severe enough to cause death immediately. Strokes can also cause paralysis, with 90% of stroke patients experiencing some form of paralysis.” The aftereffects of Dr. Dyi’s stroke are mild in comparison. “I cannot talk the way I used to talk,” she says, “I talk and forget what I was saying or was going to say. My training is in medicine, and sometimes if I want to say a long medical term, I just can’t do it.” The stroke also seems to have affected one of her legs, but you can’t tell by looking at her. “A doctor is a doctor’s worse patient,” she explains, “So when the doctors told me to wear a brace, or use a cane, I just wouldn’t. I didn’t want anyone to know I had a stroke.” Dr. Dyi’s advice to individuals who have high blood pressure: “Don’t ever skip your medication. Don’t be scared to call a doctor. Ever!”
Healthy eating is also high on her list of things to do: “We all have smart phones,” she says, “There are all kinds of apps that will help you select the right foods. You don’t have to diet, just flood your refrigerator with healthy foods. Instead of a hamburger, grab an apple.”
Exercise is also important. Dr. Dyi walks for thirty minutes every day after dinner. According to Harvard Medical school, “Lack of physical activity makes you more prone to having a stroke. People who are physically active are 25% to 30% less likely to have a stroke than inactive people.” Current federal guidelines recommend 150 to 300 minutes per week of moderate aerobic exercise such as brisk walking or 75 to 150 minutes a week of vigorous exercise, such as running, or a combination of the two, in addition to two or more strength training sessions per week. Always check with your doctor before beginning an exercise program.
It is understood that people with high blood pressure should watch their salt intake. Read labels and stay away from foods with high sodium content.
That goes for sugar also. Cakes, pies, and cookies should not be a regular part of your diet.
Dr. Dyi also recommends monitoring your blood pressure at home. (Blood pressure monitors cost around $30 or $40 or less and are free with some insurance plans.) Dr. Dyi tells us she takes her blood pressure at least once a week. “It should be around 120/80, ideally, and if it goes up to 140, then I will watch it more closely—then I might go from once a week to every other day. If it stays high, then you need to talk to your doctor,” she says.
A healthy lifestyle and the right blood pressure medication can make the difference between being a success or a statistic.